The steps are as follows:
1) 1. The patient is positioned face down with the head to one side, with a pillow under the abdomen to reduce the spinal curve, and the feet turned outward to facilitate access to the peridural space.
2) Patient’s vital signs are monitored.
3) The point of entry is sterilized.
4) Local anesthesia is administered at the point of entry. It can be delivered by inserting a needle deeply through the muscles until it reaches the bone.
5) Confirmation through x-rays of the correct position of the needle, in both anteroposterior and lateral views. After negative aspiration for blood or CSF, the contrast substance is injected.
6) The catheter is introduced through the needle. Bending the tip of the catheter approximately 15º, can make it easier to reach the target area. Sometimes various attempts are required before the catheter reaches the fibrous tissue.
7) Once the target is reached, negative aspiration is performed and 5-10 ml of contrast is administered through the catheter. This allows us to see where the contrast extends and where it does not, so that we can detect which part of the epidural space has the highest degree of fibrosis and which roots are most affected.
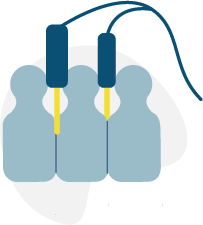
8) At this point, it is also possible to perform pulsed radiofrequency on the dorsal node of the affected root through the epidural space. For this, the Racz catheter is connected by means of a crocodile clip to the radiofrequency apparatus and the usual procedure is followed of sensory stimulation at 50 Hz and motor stimulation at 2 Hz with an adequate impedance. Pulsed lesion is performed for between 4 to 8 minutes.
9) At this time, 1,500 IU of hyaluronidase dissolved in 4-10 ml of sterile isotonic saline is administered, followed by a slow, fragmented injection of 10 ml of ropivacaine 0.2% or levobupivacaine 0.25%, along with the corticosteroid, preferably 40 mg triamcinolone acetate.