The implantation process for deep brain stimulation consists of a single surgery to insert the components of the electrodes and battery. The patient is given approximately 3 to 6 weeks to allow for sufficient recovery.
At Instituto Clavel, we perform the stage 1 procedure with the patient under general anesthesia, unlike some other centers where this procedure is performed with the patient awake. We are able to complete this procedure in 3 hours. Due to the advance planning of high-resolution images and neuronavigation, intracerebral monitoring is not needed during this surgery, allowing us to shorten the surgical time, and it is as safe, or safer, than performing the same surgery using intraoperative neurophysiological monitoring. Working this way, we achieve more effective results and there are fewer complications.
In this first stage, electrodes are implanted in specific areas of the brain. The patient's head is placed in a special frame with small screws to immobilize it for the duration of the procedure. Sometimes the procedure is done with an MRI and a frame is used above the head instead of around it.
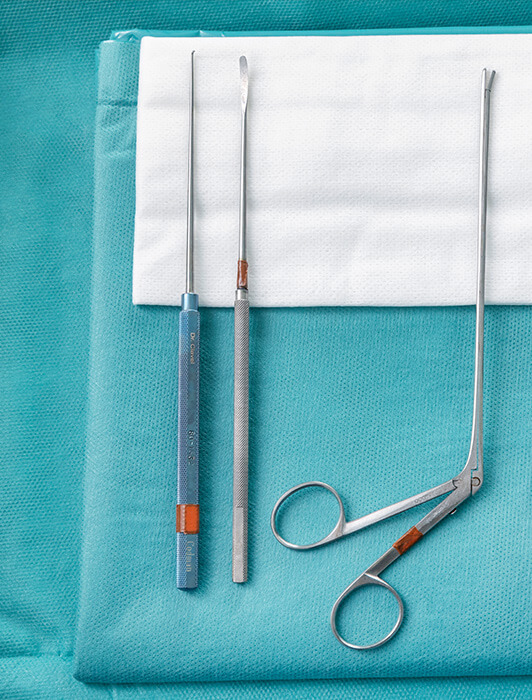
The surgeon will drill a small opening in the skull and place the lead in a specific area of the brain. (If both sides of the brain must be treated, the surgeon will make an opening on both sides of the skull and insert two leads.)
Small electrical impulses will be sent through the lead during the procedure so that the surgeon can check that the electrodes are properly connected to the area of the brain responsible for the patient's symptoms.
In Stage 2, the patient is also under general anesthesia. It is in this phase that the pulse generator, or "brain pacemaker", will be implanted.
The surgeon makes a small incision, in most cases just below the collarbone, and implants the neurostimulator. It is placed under the skin of the thoracic area, near the collarbone, and will be connected with wires to the electrodes that were implanted in Stage 1.
Once connected, the surgeon closes the incision. As the neurostimulator and wires are inserted just beneath the skin, there may be a small, visible bump. Once the wires have been connected, they transmit electrical impulses from the neurostimulator directly to the brain. These impulses interfere with and override the electrical signals that cause the symptoms of some diseases.