The technique consists of two parts: first, the approach, and second, the arthrodesis itself.
APPROACH
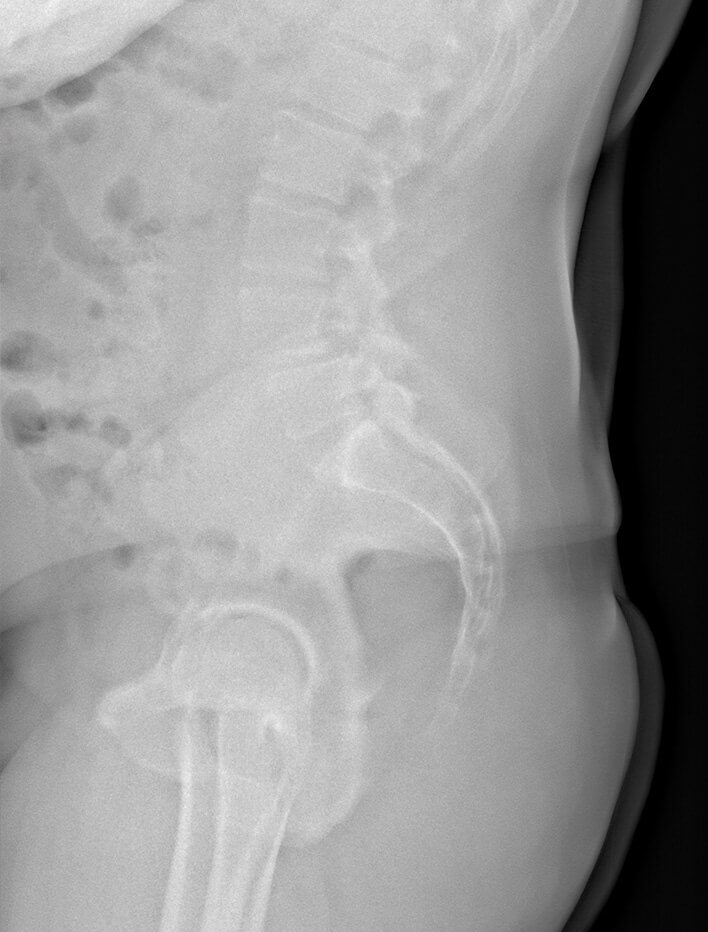
With the patient lying on one side, the surgeon makes a lateral incision, usually horizontally, to access the muscles of the abdominal wall. Next, the muscle fibers are separated (without cutting them) from the external oblique, internal oblique and transverse muscles of the abdomen. Once past the transverse muscle of the abdomen, the retroperitoneal space is accessed, where the psoas muscle is identified. Using specific instruments, we pass through this muscle, performing neurophysiological mapping to identify the nerves in the muscle so as not to harm them. A separator is then placed that allows us to access the intervertebral disc.
ARTHRODESIS
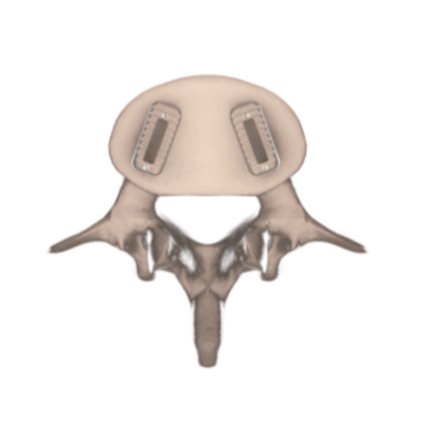
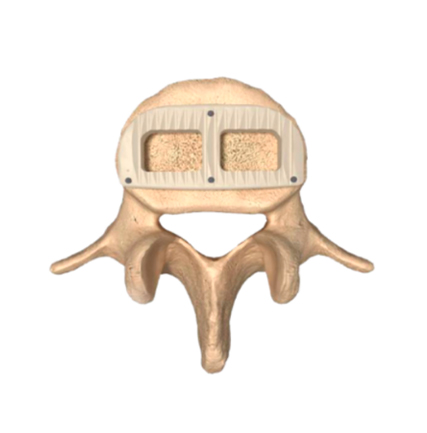
The diseased intervertebral disc is cut out. Usually, this access is used for the upper lumbar segments up to L4-L5, except for the L5-S1 space. Once the disc is completely removed, the vertebral endplates are cleaned, removing the cartilage, so that the arthrodesis material can more easily contact and fuse with the bone of the vertebra. Once the disc space has been prepared, the interbody fusion cage, or “spine cage” can be placed (it can be made of a variety of materials such as titanium, porous titanium or PEEK- Polyetheretherketone, titanium-coated PEEK, NanoMetalene etc..).
These materials have the characteristics of driving the fusion, that is to say, they guide the formation of the bone callus between the two vertebrae. Usually, to facilitate the formation of this callus, the “cages” are filled with a material referred to as bone wax, which may be of various origins. These are biological materials, which, in addition to helping and guiding the formation of the callus, they generate and stimulate formation of bone. After the fusion takes place, the surgery is usually completed with the placement of posterior screws that will be implanted in a minimally invasive percutaneous way, to give greater stability to the fused vertebrae.