With brain and cranial surgery, we refer to all the surgical techniques aimed at treating the brain mass and its attached organs, including the cranial bone vault, the meninges, the cranial nerves and the pituitary gland.
Acabar con el dolor es posible y nuestro equipo quiere ayudarle a conseguirlo. Dé el primer paso contactando con nosotros.
Madrid: +34 919 148 441
Barcelona: +34 936 090 777
Llevamos la excelencia neuroquirúrgica a Sevilla, ofreciendo servicios especializados en neurocirugía de columna y cráneo.
¡Llama al +34 955 277 751 o +34 633 143 686 para más información!
With brain and cranial surgery, we refer to all the surgical techniques aimed at treating the brain mass and its attached organs, including the cranial bone vault, the meninges, the cranial nerves and the pituitary gland.

In cranial neurosurgery, we treat a wide range of pathologies, with a variety of origins, and different levels of severity and consequences for the patient. We can classify these surgeries according to the pathology to be treated, creating different subspecialties that we offer at Instituto Clavel:
Treatment of tumors (neoplasms) of any origin and degree of aggressiveness, including primary tumors of the central nervous system (gliomas, oligodendrogliomas, schwannomas, etc.), metastases (satellite tumors of pre-existing malignant tumors of any origin outside the nervous system), tumors of the meninges (meningiomas), among others.
Generally, surgery to remove tumors located at the base of the skull. This is an anatomically very complex bone structure with multiple, difficult to access, entrances and exits of important nerves and blood vessels. There is a series of specific techniques used to surgically access these locations. This category of surgery overlaps with some areas of functional neurosurgery, for example, cranial nerve surgery.
Aimed at treating the pituitary gland, which is located at the base of the skull in an area bordering on the paranasal sinuses and nostrils. It is a specific type of skull base surgery.
Aimed at treating congenital or acquired vascular malformations, such as arteriovenous malformations (AVMs), brain aneurysms, and cavernomas.
Indicated for malformations involving high vertebral instability or compression of the medulla or cerebellum at its exit from the skull (Chiari malformation).
Used for both congenital and acquired disorders that can give rise to problems in the natural circulation of the CSF, especially its reabsorption, causing it to accumulate in excess inside the brain (hydrocephalus) and creating endocranial hypertension, so that surgical bypass techniques are required to facilitate evacuation of the fluid.
Surgical treatment intended to control neuropathic pain (neuralgia) of cranial nerves like the trigeminal nerve.
Focused on the evacuation of intracranial or intrabrain hematomas, sunken or unstable skull fractures, or massive brain edema of traumatic origin.
For those cases where there is a major cosmetic defect in the cranial vault due to injury or following removal of a cranial tumor, reconstructive surgery can be done using custom-made implants to restore the skull to its original shape.
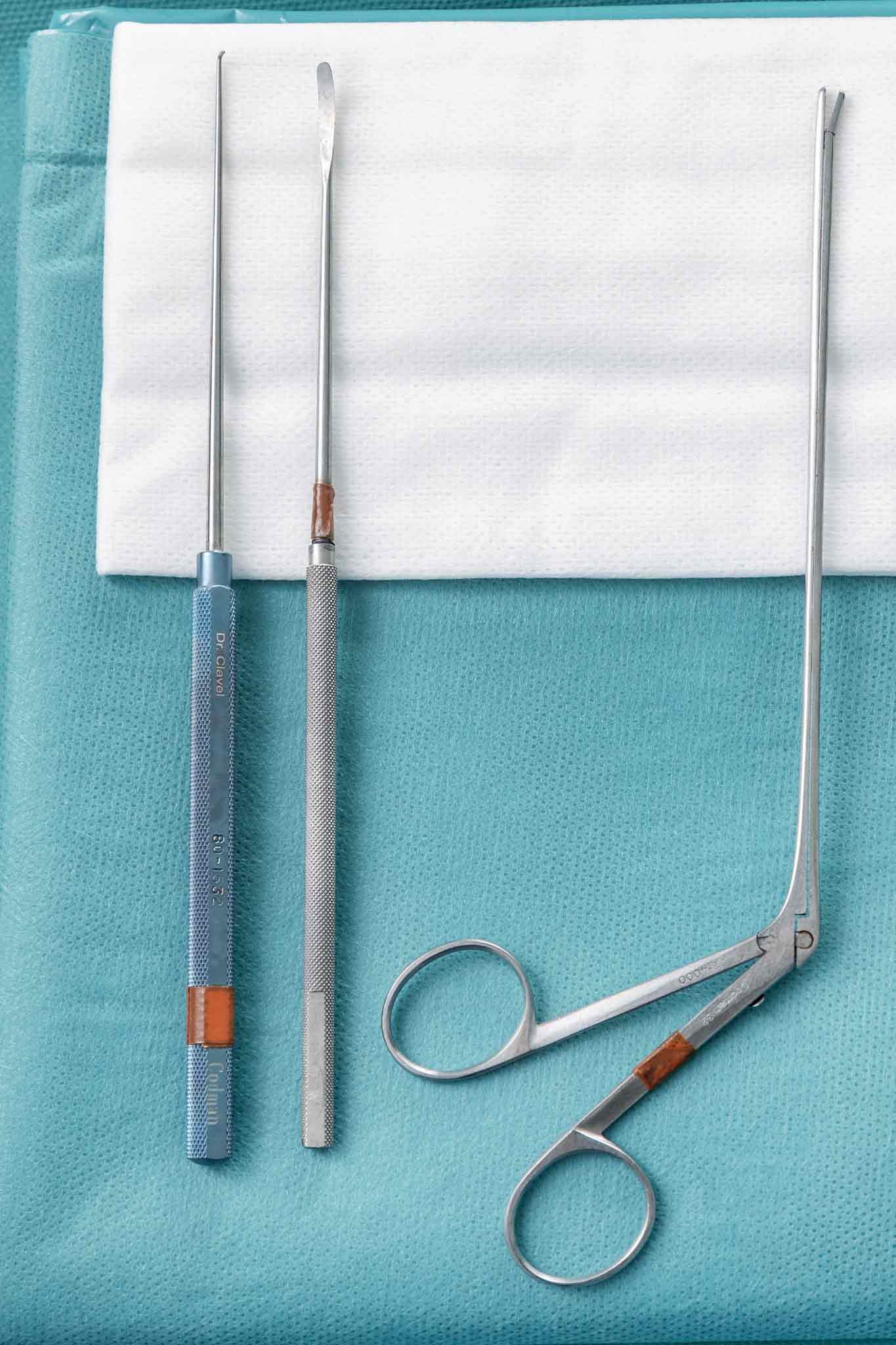 Brain surgery typically begins with the process of opening the skull to access the location of the pathology to be treated. This can be achieved by practicing a simple hole in the bone using a tiny blade (trephine) or by making a window in the bone and lifting a bone fragment that will be returned to its position at the end of the surgery (craniotomy), or not (craniectomy), as required in the specific case.
Brain surgery typically begins with the process of opening the skull to access the location of the pathology to be treated. This can be achieved by practicing a simple hole in the bone using a tiny blade (trephine) or by making a window in the bone and lifting a bone fragment that will be returned to its position at the end of the surgery (craniotomy), or not (craniectomy), as required in the specific case.
Using the trephine procedure, it is possible to evacuate some hematomas located between the brain and the skull bone (subdural hematomas), place catheters for the evacuation of cerebrospinal fluid and the treatment of hydrocephalus (ventricle-peritoneal shunt), and even perform the biopsy of intrabrain tumors.
A craniotomy is the technique used when we need greater control of the situation. After lifting the bone we find the dura, the thickest of the three membranes that cover the brain (meninges), which we will also then open to access the brain tissue. In some specific pathologies, such as the Chiari malformation, by this action we will have already achieved the decompression of the anatomical element that is the object of the operation.
In the case of some tumors and some vascular lesions, such as AVM and cavernomas, the goal is to completely or partially remove the tumor or lesion, depending on the function of the anatomical structures affected, and the degree of malignancy in the case of tumors.
In the case of brain aneurysms, (malformation in the wall of the brain arteries with high risk of bleeding and brain hemorrhage), the objective will be to place a small clip that will strangle and collapse them, thus preventing their rupture and bleeding, and returning the blood flow to its correct path.
There are many types of cranial and intracranial pathologies, each with its own particularities, depending on the exact anatomical location, the neurological symptoms it causes, the degree of aggressiveness of the pathology, and the general condition of the patient, including other diseases. Therefore, each case is planned individually according to the needs and situation of the patient.
There are some specific technological tools that help us carry out these surgeries with greater safety and precision. For example, we use neuronavigation, guided by the patient's imaging tests and anatomical references, which aids in getting the precise location of the lesion, so we can adjust the size and location of the craniotomy, and take it into account in the pre-surgery planning and performance of the operation.
A surgical microscope is also routinely used to get a better view of the small, fragile structures.
In some cases, contrast and fluorescence techniques with compounds such as 5-ALA (Gliolan) are used under the microscope to optimize the identification and degree of resection of malignant neoplasms.
Additionally, other techniques are also sometimes used, such as intraoperative brain ultrasound to locate tumors in real time, or endoscopy to access deep and otherwise inaccessible locations.
In addition, intraoperative neurophysiological monitoring is routinely used in brain surgery. Thanks to this technology, the neurophysiologist is able to track the brain activity in real time of any structures possibly at risk, giving the surgeon and anesthetist greater knowledge of what is happening during the surgery, detecting problems that need attention, and alerting of dangerous events before they occur, thus preventing lesions or neurological after effects. Since the advent of this technique, the negative repercussions of this type of surgery have been dramatically reduced.
Except in cases of minor skull perforations (trephines), the patient is routinely transferred to the ICU for optimal neurological, hemodynamic, and respiratory control after surgery.
If the post-surgical recovery goes as expected, within 12- 14 hours after the surgery the patient will be transferred to a hospital room where he will begin to sit up and move about with the help of the nursing staff and physiotherapists.
The length of hospitalization will depend on the patient’s ability to move about and perform routine activities of daily life. This means that it can be between a single night in the hospital following ventriculo-peritoneal bypass surgery, to a week in the case of tumors with large neurological impact, which will require more assistance. In general, the average hospital stay needed for a craniotomy is between 4 to 5 days.
After surgery, patients who notice weakness in the limbs, or have difficulty walking normally due to problems of coordination or balance, will benefit from a personalized rehabilitation plan until they are able to return to the maximum possible functionality given their individual case. If the patient notes any change in the ability to swallow or alterations of speech, it is advisable to see a speech therapist.
A patient who does not suffer any limiting neurological deficit and who does not require additional treatments (chemotherapy, radiotherapy, etc.) could return to normal activity in about 6-8 weeks.
In general terms, any brain surgery can be complicated by severe intracranial hemorrhage in the first 48 hours, its frequency having been described as 1% of cases. Likewise, it is estimated that around 2% of cases will suffer an infection of the surgical wound.
Each type of pathology and, depending on the location of the pathology, presents a specific type of neurological risk, with different possible functional alterations and degrees of severity.
Therefore, we inform each patient of the estimation of risks for their specific case, depending on the type of pathology, the anatomical location of the problem to be treated, their medical history and the type of surgery to be performed, so that they are fully informed before consenting to surgery.
This type of surgery is performed exclusively by specialists in neurosurgery. In our team, Dr. Montes is responsible for brain pathology.
Contact us so that we can give you a personalized assessment.